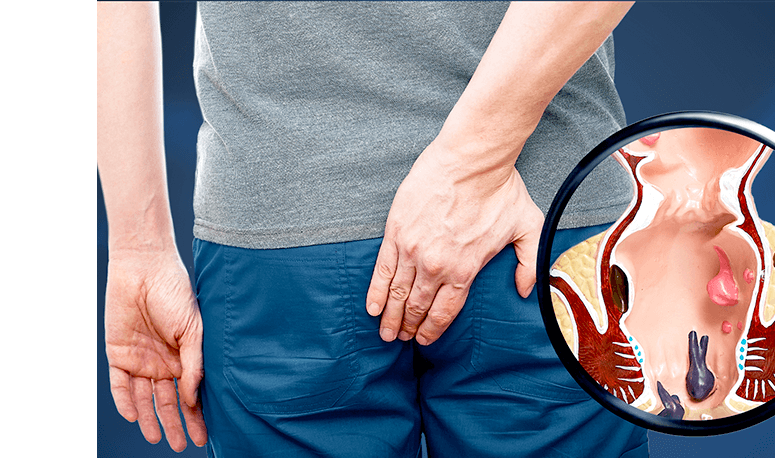
Anal Fistula Repair & Surgery
An anal fistula generally requires specialised treatment for recovery, including surgery, as it typically does not heal properly on its own and can be very uncomfortable.
How Is Anal Fistula Treatment Determined?
It primarily depends on the location and complexity of the anal fistula. Fortunately, most fall into the category of simple fistulas (e.g. only one tract; does not pass through the sphincter muscles) and are straightforward to treat.

Common Surgical Treatments for Anal Fistula
The main goal of surgery is to allow the anal fistula to heal while minimising any impact on the nearby anal sphincter muscles (so as to retain bowel continence). Different types of anal fistula surgeries are recommended based on how deep or complex the fistula is. Common types include:
Fistulotomy
The most common method is a fistulotomy, whereby the anal fistula is cut and laid open, allowing it to drain and heal from the inside out as a flat scar. It is often used for simple, low-lying fistulas that do not involve much of the anal sphincter muscle. With a high success rate and minimal risk of recurrence, fistulotomy is one of the most effective treatments for anal fistulas.
Seton
A seton is a thread or rubber band that is inserted into the anal fistula. It helps drain the infection and gradually cut through the fistula tract, allowing it to heal over time. This procedure is commonly used to protect the sphincter muscles from complex or high fistulas. A second procedure (fistulotomy) may be required.
Bioprosthetic Plug
Alternatively, a bioprosthetic plug is a cone-shaped plug inserted into the fistula tract to block the openings, allowing the surrounding tissue to heal naturally. While it is a less invasive option, it may not be suitable for all types of fistulas. This option is often used for complex fistulas that cross the anal sphincter muscles, particularly when other surgical options have failed.
LIFT
The Ligation of Intersphincteric Fistula Tract (LIFT) technique is used for fistulas that pass through the internal sphincter muscles. It involves the removal of infected tissue and the closure of the anal fistula’s internal and external openings. This procedure is suitable for complex or high fistulas and aims to minimise the risk of damage to the sphincter muscles and potential incontinence.
While these procedures are effective treatments for anal fistula, they often come with risks such as incontinence, longer recovery times, and scarring. For those seeking a less invasive option, laser anal fistula treatment offers an advanced and promising alternative.
How to Prepare for Anal Fistula Surgery
Preparing for anal fistula surgery is essential for ensuring a smooth and successful procedure. Proper preparation typically entails:
- Pre-surgery Consultation - The surgeon will thoroughly review the patient’s condition before the surgery. Diagnostic tests, such as blood tests or ultrasound, may be conducted.
- Bowel Preparation - To reduce the risk of infection, a bowel cleanse may be instructed. This may involve the use of laxatives or enemas to empty the intestines, especially for surgeries involving deeper or complex fistulas.
- Medication Adjustments - The patient may be advised to adjust or stop certain medications before the surgery. This commonly includes blood thinners like aspirin, which can increase the risk of excessive bleeding.
- Fasting - As with other surgical procedures, patients must typically fast for 6 to 8 hours before the surgery.
- Lifestyle Adjustments - Smoking and alcohol consumption should be avoided as they can interfere with wound healing. Sufficient rest is needed to help the body conserve energy and prepare for the demands of the surgery.
We strive to provide effective and tailored anal fistula treatments for every patient.
Recovery Process After Anal Fistula Surgery
During the initial postoperative period, minor drainage of pus or blood is normal. Adhering to prescribed medications and keeping the surgical site clean and dry is crucial. Early bowel movements tend to cause mild discomfort, but this usually resolves itself over time. A high-fibre diet softens stools to reduce strain, while sitz baths after bowel movements can provide relief.
Most patients may resume work within 1–2 weeks, but strenuous activity, heavy lifting, and prolonged sitting should be avoided as advised by the surgeon. Regular follow-ups are essential to monitor healing and address complications, depending on the fistula’s complexity. Depending on the fistula’s complexity, full recovery can take several weeks to months.
Potential Complications of Anal Fistula Treatment
Surgical success rates for anal fistulas are high, with most patients making a full recovery. However, there is a small risk of complications, including:
- Persistent Pain and Discomfort
- Recurrence of Anal Fistula or Abscess
- Faecal Incontinence
- Fistula Tract Damage
Frequently Asked Questions
How can I prevent an anal fistula?
Preventing anal fistulas involves maintaining good perianal hygiene, consuming enough dietary fibre, staying hydrated, not delays in bowel movements, and promptly treating anal issues.
Is anal fistula surgery the only way to treat the condition?
While antibiotics and home remedies may offer temporary relief, surgery is generally the most effective and lasting treatment for anal fistulas.
Can an anal fistula heal on its own?
No, anal fistula cannot heal on its own. Small or less complex anal fistulas may improve with conservative treatments like antibiotics and drainage. However, surgery is usually necessary to treat the condition fully.

Dr Dennis Koh
Medical Director & Senior Consultant Surgeon
B Med Sci (Nottingham), MBBS (Nottingham)
MMed (Surgery), FRCS (Edinburgh), FAMS
Dr Dennis Koh is an MOH-accredited and experienced colorectal surgeon skilled in anal fistula treatment; and currently the Medical Director at Colorectal Practice.
Dr Koh strives to provide a customized treatment plan for each patient, which allows for better outcomes. He also honed his skills in proctology abRd in Geneva, bringing a more diverse touch to his practice.

Dr Sharon Koh Zhiling
Senior Consultant Surgeon
MBBS (Singapore), MMed (Surgery),
FRCS (Edinburgh), FAMS
Dr Sharon Koh is an experienced colorectal surgeon and the former Director of Endoscopy at Alexandra Health.
Dr Koh completed her fellowship at Cedars-Sinai Medical Centre in the US after being awarded the Academic Medicine Development Award by the National University Hospital.

Dr Pauleon Tan Enjiu
Senior Consultant Surgeon
MBBS (Singapore), MMed (Surgery),
FRCS (Edinburgh), FACS
Dr Pauleon Tan has served in public hospitals for over 15 years and is experienced in minimally invasive surgery and endoscopy.
Dr Tan undertook advanced colorectal surgical training at Japan’s Saitama International Medical Center after being awarded the Ministry of Health – Health Manpower Development Plan (HMDP) Award.